All you need to know about
Shoulder instability
Why should you, as a patient or future surgeon, inform yourself? It’s about you and your shoulder.
Available soon…
You are the principal actor of your surgery
You will be the only one present from the beginning to the end of the care process, from A to Z and beyond that, you’ll have to live with it. In other words, you need to be part of the project, part of the surgical team. To feel at ease within this team, it’s essential to inform you and give you the keys to communicating as well as possible with the caregivers.
Why do I need shoulder stabilization surgery?
Shoulder stabilization surgery is most often proposed to treat recurrent
dislocations (dislocation or loss of contact between joint surfaces). Recurrent
shoulder dislocation is defined as the occurrence of two or more shoulder dislocations in the course of a lifetime
.
More rarely, surgery is proposed after a single episode of dislocation if this is associated
with significant bone damage, or if the patient practices high-risk sports or at
high level.
However, there is the special case of dislocation after the age of 40, which is accompanied by a
rotator cuff lesion in one case out of two, which also justifies an operation
to repair the ruptured tendons (see “my rotator cuff & me” booklet).
In order to help the surgeon in his decision making, prognostic scores (ISIS score) can
be used to define the potential risk of dislocation recurrence?
Surgical treatments
It’s a question of choosing which of the various existing techniques is best suited to your situation. The surgeon will correct the morphological lesions observed during the imaging workup. For example, the surgeon may decide to act on the glenoid bulge in isolation, or on a bone lesion on the glenoid or humerus, or to combine several procedures in the same operation if he or she so wishes, thus creating a truly “à la carte” treatment. The aim is to adapt the treatment to the lesion.
The main procedures performed :
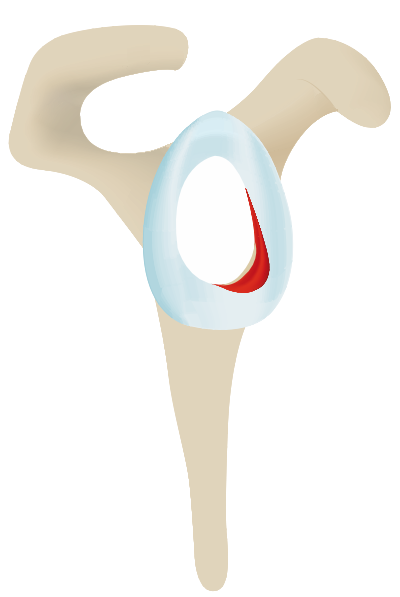
The “Bankart” operation
Involves repairing the glenoid bead. The joint capsule is usually retensioned at the same time. Anchors with or without knots are used, depending on the surgeon’s preference.
Hill Sachs Filling
This is an operation designed to fill the bony notch in the posterior part of the humerus with the infraspinatus muscle to prevent dislocation. When combined with Bankart, this procedure is known as “bipolar locking”.
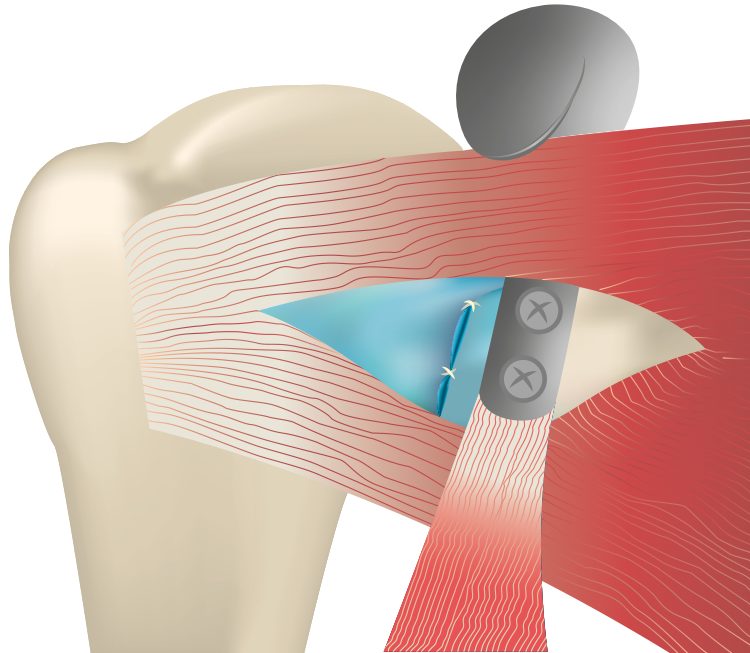
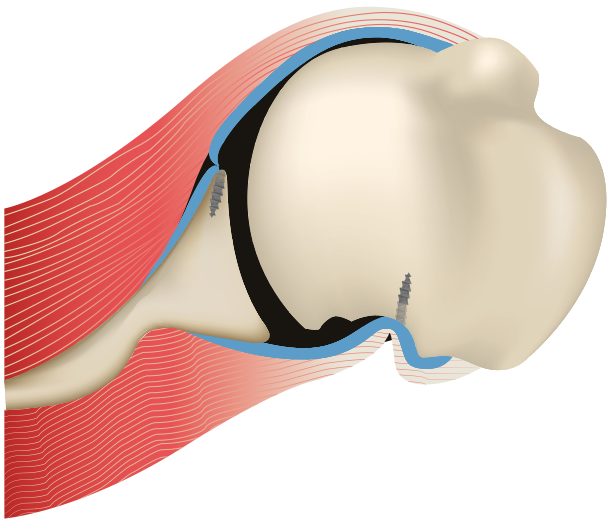
Latarjet coracoid bone block
This is the most frequently used bone block. The principle is to place a bony block at the anterior and inferior part of the glenoid to close the passage to migration of the humeral head. Imagine a snail’s head which, perceiving danger, returns to its shell. The stop acts more like this than as a mechanical obstacle. In this technique, part of the coracoid bone is harvested, with the conjoined tendon inserted at its tip, and positioned in front of the glenoid. This surgery can be performed with a small scar or under arthroscopy, and the stop can be fixed with screws or metal buttons, depending on your surgeon’s habit and preference.
Will I be able to do sports?
Physical activity is good for you. In recent years, there have been many changes in the rules governing what is and isn’t allowed. For many reasons, sport is good for :
- Your cardiorespiratory function.
- Your well-being through the secretion of euphoric substances (endorphins).
- Proprioception.
- Reinforce the muscular strength of the operated limb. Good muscles are able to absorb impact and act like springs.
The recommendations also take into account three other factors:
- A patient who performs well in a sport is more likely to return to it than one who is new to it.
- Few patients follow their surgeon’s recommendations.
- The sports recommended, tolerated or prohibited by the surgeon evolve over time, and are sometimes even influenced by the surgeon’s own sporting practice.
All these data will enable us to make individualized recommendations, as each patient’s functional requirements are different. Once again, in the majority of cases, non-armed and non-contact sports are permitted from 3 months, and contact and armored sports from 6 months. In fact, after this type of surgery, in 80 to 90% of cases, you’ll be able to play all sports without restriction, including tennis, handball and rugby, for example. Next, you need to consider the pleasure you derive from sport, the impact on your health, and the short- and long-term risks involved. The surgeon will advise you, but of course it’s all about your shoulder. So it’s a life choice. It’s only when you’re well informed that you’ll be able to make the best decisions for yourself. The aim of a sports professional is to return to full sporting activity, and the surgeon’s role is to support him or her in this quest.